Expression of stem cell markers in meningioma among Sudanese patients
Abstract
Background: Meningioma is the second most common primary intracranial tumor of the central nervous system, surgical total excision of meningioma offers a better survival to patients; however, a significant proportion of histological variant recur within 5 years despite complete excision. Chemotherapy is generally unsuccessful in treating meningiomas, so refractory and recurrence meningioma are treated with palliative surgery and radiotherapy. In this context, certain therapeutic approaches based on effective molecular biology are needed. In ecent years, the so-called cancer stem cells (CSC) have emerged; these cells can be identified by stem cell markers among many other cancers, but there is no unique marker found in all stem cells, as their phenotype varies considerably among different cells and species. The aim of the study: To characterize the RNA (cDNA) of CD 44, CD 73 and CD 105 genes as stem cell markers in meningioma among Sudanese patients and to correlate the PCR findings of CD 44, CD 73 and CD 105 genes with meningioma histological variants. Materials and methods: Using Innu PREP RNA – MiniKit (Analytic Jena) 56 tissue samples radiologically diagnosed as meningioma were immediately processed for RNA extraction and cDNA synthesis. The PCR was done using Maxime PCR premix Kit (i-Taq) entrobiotechnology. Results: This study included 56 tumor samples; 54 samples were confirmed histologically to be meningioma; 40 (74.07%) were female and 14 (25.93%) ere male. The majority of the patients were Afro-Asian (68.4), followed by Niger-Congo (22.8), and all patients had headache. CD44 was expressed in all meningioma samples (100%), CD73 was positive in 61% and negative in 39%, CD105 was positive in 89% of the samples. Conclusion: Our results showed that, the expression of cancer stem cell markers in meningioma was inconsistent within the same class of meningioma; moreover, the expression of CD44, CD73 and CD105 markers could confirm the presence of cancer stem cells in our meningioma samples.
Introduction. Meningioma is the second most common primary intracranial tumor of the central nervous system, comprising nearly 30% of all primary brain tumors with annual incidence rates 1.3 to 7.8 and mortality rate around 0.3 deaths per 100,000 individuals [1, 2].
Surgical total excision of meningioma offers a better survival to patients; however, up to 18% of benign meningioma, 40% of atypical meningioma, and 80% of malignant meningioma recur within 5years despite complete excision [3, 4]. Chemotherapy is generally unsuccessful in treating meningiomas, so refractory and recurrent meningiomas are treated with palliative surgery and radiotherapy [5, 6].In this context, certain therapeutic approaches based on effective molecular biology are needed.Still, inadequate clinical predictive power remains one of the most critical impediments in the development of novel study models [7].
The pathogenesis of the tumor is made of tumor cells and tumor microenvironment (cellular environment).This cellular environment includes the extra cellular matrix, mesenchymal stem cells, endothelial cells and signal molecules like growth factors and cytokines. There is special microenvironment that surrounds the cancerous stem cell (niche), which controls and governs the fate of this cancerous stem cell. [8]
Within the past 20 years, the so-called cancer stem cells (CSCs)] have been found [9]. They possess properties quite similar to the normal stem cells, including the ability of self-renewal and differentiation into various tumor cell subtypes.The CSCs which are a small subpopulation of cells, are capable of initiating tumor growth and metastasis; they form cancer cells in an unregulated manner, leading to carcinogenesis. [10]
These cells can be identified by stem cell markers among a variety of other cancers such as glioblastoma and colorectal cancer. Increased expression of markers of CSCs has also been associated with worsening prognosis of glial tumors, treatment resistance and higher risk recurrence and distant metastasis following chemotherapy and radiotherapy.
Stem cells which have been discovered currently by scientists have unique capabilities to self-renew, grow indefinitely, and differentiate or develop into multiple types of cells and tissues. Nevertheless, many researchers have shown existence of different types of stem cells in very small populations in the human body, one stem cell may be found in 100,000 cells in circulating blood. Microscopically these cells look like any other cell in the tissue. Hence, there are many different types of receptors that differ in their structure and affinity for the signaling molecules. Physiologically the cell uses these receptors and signal molecules which bind other cells in the body. The biological properties of these receptors have led to the emergence of the socalled stem cell markers.
These markers are known to be genes and their protein products are used by scientists to isolate and identify certain stem cells [11].In addition to that, stem cells can also be identified by a technology of functional assays which are considered the gold standard for the identification and therapeutic purposes in the future.
A number of surface and intracellular markers are described in the literature and could be routinely used for cell characterization and investigation of their stem cell phenotype [12]. Many experiments are conducted to detect a single surface marker expressed equally by all mesenchymal stem cells (MSCs). However, there is no unique marker found in all stem cells, as their phenotype significantly varies between different cells and species. Many of the surface markers applied for MSCs characterization are also used to identify CSCs. Some of the commonly used for this purpose are CD44, CD90, CD133, CD73, and CD105.
Objectives
1. To characterize the RNA (cDNA) of CD 44, CD 73 and CD 105 genes as stem cell markers in meningioma among Sudanese patients.
2. To correlate the PCR findings of CD 44, CD 73 and CD 105 genes with meningioma histological variants.
Material and Methods. This cross-sectional study was conducted at the National Centre of Neurological Sciences (NCNS), Khartoum, Sudan, during the period from 2018 to 2020. All meningioma patients attendingthe NCNSduring the above-mentioned period were enrolled in the present study. The ethical approval was obtained from the ethical committee of the Institute of Endemic Diseases/ University of Khartoum (certificate reference number: 53/2018).
Using Innu PREP RNA – MiniKit (Analytic Jena) 56 tissue samples radiologically diagnosed as meningioma were taken in sterile containers, and then immediately processed for RNA extraction within 5 minutespost-surgical excision. Around 5µ of the tumor was placed in a petri dish, and then was cut into very small pieces.After this, 450µl from RL (lytic solution) was added in a 1.5tube, then the mixture was shaken well for 3-5 minutes at room temperature, and after this, the tube was centrifuged at high speed (12000 RM) for 1 minute, then the supernatant was transferred to a new tube with spin filter- D and centrifuged at 12000 RM for 2 minutes, then the spin filter – D was discarded. Equal volume of 70% ethanol and the homogenized sample were added together in a clean test tube. Then the mixture was transferred to a new receiver tube with spin filter R, and then centrifuged at 12000 RM for 2 minutes, after centrifugation, 500 µl of HS solution was added and centrifuged at 12000 RM for 1 minute, then 750µl of LS solution was added in the filter tube and centrifuged at 12000 RM for 1 minute. The supernatant was discarded, and spin filter R was transferred to a new receiver tube. The receiver tube was centrifuged at 12000 RM for 2 minutes. Then after this,the Spin filter- R was transferred to an elution tube. Finally, 80 µl of RNase free water was added to the tube and incubated for 1 minute at room temperature.
cDNA synthesis
By using Maxime – RT PreMix Kit (intron biotechnology)10µL of RNA template and 10µl of water were added into the Maxime RT PreMix tubes (containing oligo(dT)) to a total volume of 20µL. The clear pellet was dissolved by pipetting. The cDNA synthesis reaction was done using a PCR machine (cDNA synthesis temperature 45cº for 60 minutes), the mixture was incubated at 95ºC for 5 minutes to inhibit RTase enzyme.
PCR
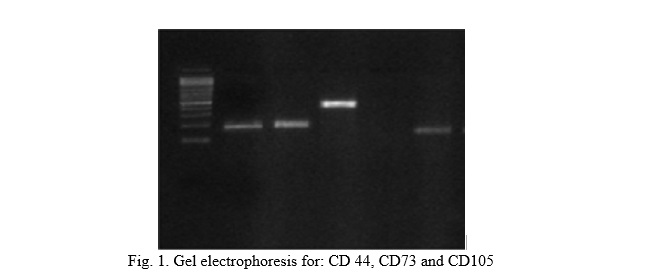
The PCR was done using Maxime PCR premix Kit (i-taq) entrobiotechnology, cDNA template and 2µLof cDNAwas added to 1 µl of (CD44, CD73, CD105), and β-actine house keeping gene, (forward and revered), + 16 µl of distil water to get a total of 20 µl. The PCR tubes were transferred to the PCR machine and amplification was carried according to the manufacturer’s protocol. Initially, denaturation at 94 ºC for 20 seconds, annealing temperature at 60 ºC for 20 seconds, extension at 72 ºC for 20 seconds, and final extension at 72ºC for 2 minutes. The PCR machine was programmed for 40 cycles to achieve a maximum PCR reaction.
Results. This study included 56 tumor samples; 54 samples were confirmed histologically to be meningioma, 40(74.07%) were female and 14 (25.93%) were male. The majority of patients were fro-Asian (68.4), followed by Niger-Congo (22.8), and all patients had headache. In this study, CD44 was expressed in all meningioma samples (100%), CD73 was positive in 61.1% of the samples and negative in 38.9%, CD105 was positive in 88.9% of the samples(Table 1).
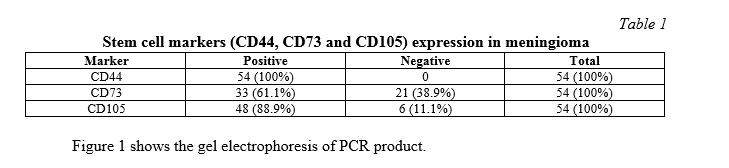
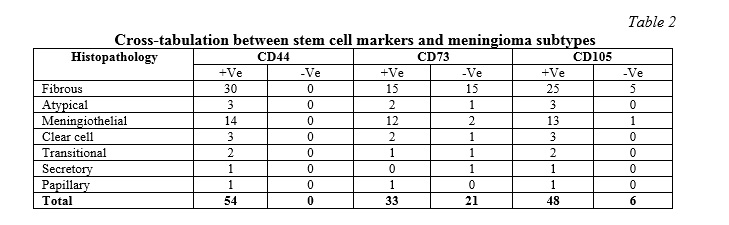
Cross-tabulation between meningioma subtypes and stem cell markers showed that all meningioma variants expressed CD44;wherease CD73 was detected in 45% of the fibrous, 6% atypical, meningiothelial 36%, clear cell 6%, and transitional and papillary 3%. CD105 was expressed in 52% of fibrous, atypical 6%, meningiothelial 27%, clear cell 6%, transitional 4%, secretory and papillary 2% (Table 2).
Discussion. The cancers stem cell (CSC) concept is supported by an increasing number of studies demonstrating the presence of subpopulations of CSCs expressing stem cell markers. Expression of such markers using PCR supported identification of such cell types to be a cancerous stem cell. However, the function of the semarkers in the context of their subcellular localization is an unexplored area of research. The identification of cancer stem cell remains unclear, and the distribution of cancer stem cells, their heterogeneity, and their relationship to tumor grade, remain uncertain. Many recent studies have addressed heterogeneity of glioma brain tumor using novel and challenging approaches, [13, 14] though, very few studies were documented for meningiomas, but interestingly, heteroregional expression was detected in grade I tumors, and particular combinations occur frequently in grade II/III.These observations could be explained by the CSC advancement hypothesis, where CSCs acquire new changes in the early development of disease and maintain new changes with disease progression [15]. One study showed heterogeneity of meningioma base on variation in expression of stem cell markers in correlation with histological variant, which may indicate aggressiveness, resistance to chemotherapy, and recurrence [16].
In the present study, we explored 3 stem cell markers in the context of their sub-cellular localization using PCR.CSCs have been proposed to be the origin of many types of cancer, including glioblastoma multiforme, tumors confined to oral cavity like squamous cell carcinoma [17, 18]. Stem cell markers CD44, CD73 and CD105, their expression and biological functions in human skull meningioma tumors are poorly understood. We aimed in this study to evaluate expression of these markers, and to determine their possible role in the tumor development and progression. Expression of the three stem cell markers in 54 meningioma samples supported the presence of stem cells in these tumors. One of the convincing markers in tumor malignancies is cluster-of-differentiation-44 (CD44) which has been reported in support of our findings as a marker for a cancer stem cell (CSC) in meningioma [19]. CD44is a transmembrane glycoprotein and is a receptor for hyaluronan 9 physiologically mediate cell and cell matrix interaction, and is found to be associated with malignancy dissemination [20, 21]. CD44 antigen is a polypeptide, encoded by CD44 gene, and consists of 19 exons located on human chromosome 11 and mouse chromosome 2 [22, 23]. Human CD44 exons 1–5 and 16–20 generate the standard structure of CD44 and the remaining exons 6–15 which are spliced to form known exonic vaiants [24].
Moreover, it is found to be the most common cancerous stem cell surface marker and plays a role in communication with micro-environment. This marker interferes with intercellular binding, migration, and angiogenesis of cancer cells [25]. In the present study, CD44 was expressed in all our samples and this may explain the aggressive biologic behavior of meningioma in Sudanese patients.
In a previous study from Sudan, Gassoomet al. reported expression of CD44immunostaining in all meningioma tissue samples studied, and higher expression was found among WHO 1 fibrous and grade 11 atypical, In the current study CD44 was expressed by all meningioma tumor grades.
A study done in Japan by Suzuki et al. [26], investigated expression of the CD44 variant (using reverse transcription polymerase chain reaction and Southern blotting) among meningioma subtypes and concluded thatCD44 is expressed in meningioma in relation to tumor cell differentiation towards the epithelial types. In our findings, CD44 expression which was demonstrated by using a polymerase chain reaction (PCR) was expressed in all meningioma sub-types. Currently, epithelial membrane antigens and cytokeratines are known to be the markers for epithelial differentiation in meningioma [27], however, expression of CD44 revealed new type of cells other than meningiothelial cells which is the meningioma cancerous stem cell.
Recently, many signaling pathways have been suggested and be important palyer in cancer progession. [28]. Purinergic signaling is a multistep coordinated cascade, including stimulated release of ATP/ADP which is hydrolyzed by the enzyme known as CD73, (ecto-5′-nucleotidase) [29]. CD73 is, glycosylphosphatidylinositol (GPI), encoded by NT5E gene, has a role in tumor immune escape and regulates cell interaction with extra-cellular matrix [30].
Moreover, uncontrolled proliferation of cancer cells needs abundance of nutrition and oxygen. High density of angiogenesis can support the nutrient for tumor cells growth. In addition, angiogenesis also plays an important role in the distant invasion of tumor cells through penetrating into immature vessels and surrounding structures.
Most meningioma (80%-90%) are benign and are classified by WHO as grade I, known as grade 1 meningioma [31]. There are 9 meningioma variants in this grade, of which meningothelial, fibrous, and transitional meningioma, are the most common variants. However, in some cases, the anatomical location of these tumor makes complete resection difficult and has decisive influence on prognosis, especially those arise in petroclival region, orbit, optic nerve and cavernous sinus, or even those encapsulate large cerebral blood vessels. Along with this, these variants can invade the dura, dural sinuses, bone or even the outer soft tissue and skin lining. Despite the limitation of surgical intervention for an unfavorable clinical outcome, those tumors are not considered typical or malignant [32].
In our study, 12 of the 14 meningiothelial subtype and 15 fibrous and one transitional expressed CD73,and these meningioma variants have the ability to invade not only the covering dura mater but the bone and skin, thus giving the cardinal features of disseminating cancer, though histologically benign tumors. Presence of CD73/NT5E on meningioma cells or on other cells within the tumor may thus be of high interest, in addition to this, the enzymatic function of NT5E which generated ADO receptors, is expected to exert other tumor-promoting functions likeinitiation of new blood vessels formation [33].
In the present study,15 out of 30 fibrous variants expressed CD73, in support of the increased vascularity encountered during resection of these tumors. Over-expression of CD73 might influence probably several basic signaling pathways. In contrast, in breast cancer where estrogen receptor (ER) was negatively regulated, loss of these receptors significantly enhances CD73 expression. Thus, CD73 is highly expressed in patients with breast cancer who are negative in estrogen receptors, and this might be promising targeting for clinical treatment [34].The incidence of meningioma has been reported to be increased in patients with breast cancer and some patients who were given hormonal replacement therapy [35]. This endogenous hormonal association may explain why not all of our samples express CD73. The most commonly used immune-histochemicalmarkers for the diagnosis of meningioma are an epithelial membrane antigen (EMA) and a progesterone receptor (PR). [36, 37]
In contrast to ER, thyroid hormones have been identified as molecules that can increase CD73 expression in several cell types, such as glioma vascular smooth muscle cells, and a ventricular myocytes cell [38, 39], but ER is not used as a routine marker for meningioma diagnosis. A significant sample in our current study expressed this marker
Furthermore, Endoglin, also known as CD105 is located on human chromosome 9. It is classified as an accessory receptor for transforming growth factor beta (TGF-β) and has been shown to be expressed on endothelial cells [40]. Its expression is up-regulated in actively proliferating endothelial cells, and has therefore been suggested as an appropriate marker for tumor-related angiogenesis and neovascularization. It plays role, as an auxiliary co-receptor for TGF-β, a pleiotropic cytokine regulating cellular proliferation, differentiation, migration and adhesion. Angiogenesis, the new formation of blood vessels from pre-existing micro vessels, is essential to numerous physiological and pathological processes. It is well known that tumor angiogenesishas a critical role in tumor progression and metastasis [41]. On the other hand,vascularization is necessary for tumor growth and metastasis, and insufficient supply of blood will render the tumor cells to undergo apoptosis/necrosis.
It was previously demonstrated that CD105-positive cells with a potential to differentiate into adipocytes and osteoblasts can be isolated from rare aggressive meningioma subtypes [42]. In this study, 48 of our meningioma samples expressed CD105. The studies in endometrial carcinoma, cervical cancer, breast cancer, esophageal squamous cell carcinoma and glioblastomahave shown that CD105 is a good marker for tumor angiogenesis [43, 44], despite CD105 expression in tumor vessels is found to be variable with cancer development [45]. In our study, 48 meningioma sample expressed CD105, and 25 out of 30 fibrous variants expressed CD105, and this may give clue of such variation in CD105 expression.
Among solid tumors, glioblastoma-multiforme displays the most angiogenic features and the highest degree of vascular proliferation and endothelial cell hyperplasia [46].Many studies have also established that the tumor vasculature creates a protective ‘microvascular niche’, within which tumor-initiating cells can resist therapy [47].The vascularity of meningiomas varies within subtypes and grades. In one study based on expression of CD105 by circulating endothelial cells in tissues undergoing active angiogenesis, such as inflamed tissues and tumors, CD105 has been proposed as a specific marker for neo- angiogenesis [48].
The expression pattern of stem cell markers, which has determined in the context of PCR results showed that CD44 was detected in all tumor types, while the expression of CD73 and CD105 markers varied among these histological subtypes. In the present study, WHO grade II showed equal expression of CD44, CD105 and CD73 in atypical and clear cell type, in contrasts to grade III Papillary highly malignant type, which showed expression of all three markers, although sample size limits conclusive evidence, this combinations of stem cell markers can be used as prognostic marker for meningioma prognosis, and is consistent with a similar result from the study done conducted by Mamber C. et al. [49]
Conclusion. The distribution of expression for individual cancer stem cell markers in meningioma was inconsistent between meningiomas same grade, but combined use and marker analysis indicate the complex spatial nature of this tumor, and it is particularly associated with higher grades. Our results show that the presence of stem cells in meningioma is confirmed by the expression of the markers CD44, Cd73 and CD105. This identification underscores and represents the key to the development and pathogenesis of meningioma.
Thanks
Authors would like to thank technical staff at the National Centre of Neurological Sciences for their valuable contribution. We acknowledge the scholars whom articles were cited in our manuscript. Also, our gratitude extends to all editors and publishers of journals and books for their contribution in the research area of cancerous stem cell















Reference lists