Effect of Cigarette Smoke on Female Reproductive System: A Sytematic Review
Abstract
Background: The closest toxic exposure is cigarette smoke, and nowadays smokers are not only men but also women. Although the number of smokers has dropped, cigarettes remain to be an element in the development of many illnesses. Cigarette toxic substances can disrupt cellular balance, including in the reproductive system. The aim of the study:To find out more about the effect of smoking on female reproduction. Materials and methods: Articles were searched in Google Scholar, Sciencedirect, Frontiers, Pubmed and Cochrane databases between 2014-2024 with the keywords "cigarette smoke, e-cigarette, nicotine, female reproductive system, uterus, endometrium, oviduct, ovary, estrogen, folliculogenesis, angiogenesis, and GnRH." Eighteen articles met the inclusion criteria. Results: This research is a literature review with articles selected through inclusion criteria. The results of the data analysis showed an increase in MDA, apoptosis, VEGF, iNOS, and COX-2, as well as a decrease in the number of ovarian follicles, CYP19, YAP, GnRH, AMH, FSH, LH, estradiol, SOD, GPx, CAT, thinning in oviduct thickness and oviduct mucosal folds. Conclusion: Smoke of cigarettes has a variety of harmful effects, including ovotoxicants. Smoking tobacco increases oxidative stress, causes inflammation, increases apoptosis leading to follicle loss, and decreases the synthesis of estrogen, GnRH, FSH, LH, progesterone and estradiol. All this affects female reproduction. There is evidence that smoking disrupts the regulation of reproductive hormones, which affects decreased reproductive functions of the ovaries, uterus, and ovaries. Although it does not affect in vitro fertilization, smoking should still be avoided due to its harmful effects on reproductive cells and hormonal balance. Therefore, given the harmful effects associated with reproduction, it is expected that smoking patterns will decrease
Introduction. Smoking is known to be one of the factors of premature death that can still be prevented in the world [1]. The prevalence of smoking in adolescents from 2008 (27.7%) to 2021 (9.8%) is known to have decreased. More than 75% of men who smoke every day live in countries with a medium or high Human Development Index (HDI), while more than 53% of women who smoke regularly every day live in countries with a very high HDI. Though historically low, the majority of low HDI countries have a relatively low smoking prevalence – tens of millions of people still smoke. In extremely high HDI nations, the prevalence of female smoking peaked a few decades after that of male smoking, but in the majority of low-, medium-, and high HDI countries, it has either remained relatively low or has only moderately increased thus far [2]. The survey from 2011-2022 also showed the fastest decline in cigarette users at the age of under 40 (19.2% to 4.9%), especially in those with high incomes [3]. Although the global prevalence of smoking is declining, smoking remains a major health problem in the world [4].
The types of cigarettes currently circulating are conventional cigarettes and electronic cigarettes. Conventional cigarettes are known to have high toxicity [5]. CS induces proinflammatory cytokines interleukin-8 (IL-8), interferon gamma (INF-γ), interleukin β (IL-1β), tumor necrosis factor (TNF-α), inter-leukin 2 (IL-2) interleukin 6 (IL-6) leading to disease progression [6]. E-cigarettes are often considered a safe substitute for conventional cigarettes [4]. E-cigarettes contain nicotine and flavor variations that can increase toxicity significantly [7]. The heat generated initiates oxidation and breaks down the components in it and ultimately forms harmful elements when inhaled [8]. Even so, both have the same carcinogenic and toxic risks [9].
Cigarette substances including cadmium (Cd), tar, nicotine, benzo a pyrene (BaP) induce an increase in ROS and cause oxidative stress [10]. Characterized by an increase in malondialdehyde (MDA) and a decrease in catalase (CAT), superoxide dismutase (SOD), and glutathione peroxidase (GPx). The process through which ROS accumulate in cellular macromolecules results in biomolecular damage, including lipid peroxidation in cell membranes, ATP depletion, and damage to deoxyribonucleic acid (DNA), which is quantifiable by amounts of MDA. Meiotic DNA and amino acids are reacted with by chemically active MDA during the production of proteins. Because both aldehyde groups are reactive with nucleophiles, MDA can generate adducts that harm lipids. Additionally, MDA and ROS, one of the mediators of cell functional abnormalities, have a favorable relationship [11].
Smoking causes modifications to the cell membranes of lipid sections, induces inflammation, and vasomotor dysfunction that can lead to impaired cellular function [12]. Cigarette smoke directly damages mitochondrial respiration resulting in impaired ATP production [13]. As a result, the distribution of ATP is disrupted and the cell stops working and then undergoes death [14]. Cell death disrupts the body's homeotasis and inhibits the metabolic processes that take place [15]. In addition to active smokers, passive smokers who are exposed to cigarette smoke also have the opportunity to experience the same pain [16]. The impact of smoking in health can increase the risk of cardiovascular disease, atherosclerosis, impaired kidney function, pulmonary emphysema, and hormonal disorders [17]. In addition, cigarettes are also known to have an impact on reproductive health by resulting in disorders of the oviduct, uterus, and ovaries [8].
The aim of the study. This article aims to further review the impact of cigarette smoke on the reproductive organs, especially the ovaries, oviduct, and uterus.
Materials and Methods. Research articles obtained from Google Scholar, Cochrane, Frontiers, and Pubmed databases with the keywords "cigarette smoke, e-cigarette, nicotine, female reproductive, uterus, endometrium, oviduct, ovary, estrogen, folliculogenesis, angiogenesis, and GnRH". Articles reviewed are free-access articles only. The inclusion criteria are articles in 2014-2024, true experimental, quantitative research, and complete. The exclusion criteria are literature review, narrative review, and systematic review (Fig. 1).
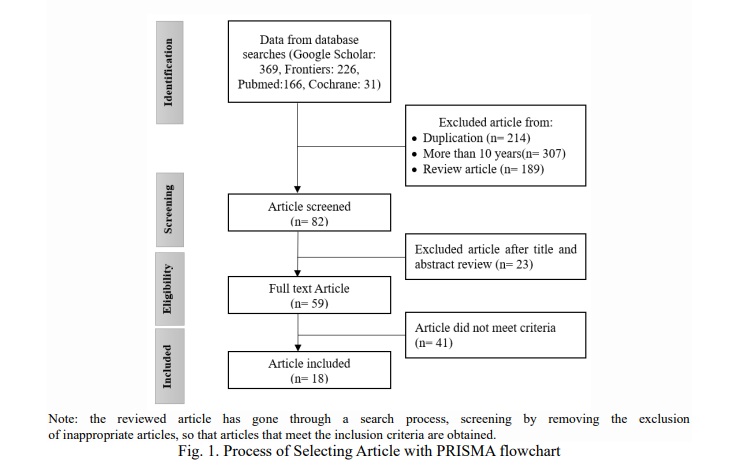
The search yielded a total of 792 articles, of which 710 were omitted due to known duplicates, review articles and articles older than 10 years. There were selected full-text articles related to the effects of smoking on female reproduction. The articles obtained are in accordance with the inclusion criteria.
Results. We studied 18 articles from 2014-2024 that discussed the effects of smoking on female reproduction (Table 1). All were laboratory experimental studies with rat subjects (44.4%), mice (11.1%), and human tissue (44.4%). Materials to assess the effects of cigarettes were e-liquid (5.5%), cigarette smoke extract (11.1%), nicotine injection (16.7%), and cigarette exposure (66.7%). All types of cigarette exposure are ovotoxicant, that is, they interfere with the normal development of follicles by decreasing the number of normal follicles, granulosa proliferation index, CYP19 and YAP expression, and serum AMH, and increasing the follicular apoptosis index especially in theca, HSCORE, iNOS expression, and COX-2. Exposure to cigarettes resulted in a decrease in antioxidants (SOD, CAT, and GPx) and an increase in markers of oxidative stress (MDA). In the fallopian tubes, smoking leads to thinning of the mucosa and degeneration of epithelial cells.In the endometrium, smoking causes a decrease in proliferation and increase in cell death. In addition, it also causes a decrease in the secretion of GnRH, estrogen, FSH, LH, progesterone, and estradiol.
Discussion
Cigarette Smoke against Ovaries
The toxicity of cigarettes can lead to abnormalities at the cellular level, in tissues and in organs [36]. The accumulation of cigarettes in the body triggers an excessive increase in ROS and causes an imbalance called oxidative stress [24]. The mechanism of increased ROS in cellular biomolecules causes biomolecular damage that triggers the formation of malondialdehyde (MDA) [37]. As a substance that can characterize the activity of free radicals in cells, malondialdehyde (MDA) is a useful tool for identifying oxidative stress brought on by free radicals. The reactivity of both aldehyde groups to nucleophiles allows MDA to form additions that result in damage to lipids and become mediators of reproductive disorders [38].
Ovarotoxic nicotine can damage the structure of ovarian cell membranes due to low FSH stimulation of follicles, causing follicles to atrophy and eventually degenerate [39]. Low FSH levels trigger FOXO to enter the cell nucleus and induce apoptosis by releasing BCL2 and FAS ligands. Furthermore, damage occurs to mitochondria, which results in the release of cytochrome C. Cytochrome C will bind to Apaf-1, which causes the apoptosome to modulate caspase 9 into caspase 3, resulting in DNA fragmentation and apoptosis. As a result, follicles are damaged in folliculogenesis and DNA oxidation occurs in follicles and corpus luteum [40].
Yes-associated protein (YAP) plays an important role in hippocampus signaling to trigger granulosa cell proliferation (GCs), maintenance of normal ovarian function, and follicle development, which is known to decrease when exposed to cigarettes [18]. A decrease in YAP followed by a decrease in CYP19 will inhibit estrogen synthesis [41]. In addition, cigarettes induce the production of pro-inflammatory cytokines such as TNF-α, NF-kB, IL17A, and IL1B [42]. Necrosis, as one of the inflammatory responses, results in plasma membrane rupture and lysis, as well as spillage of intracellular contents into surrounding tissues causing tissue damage [43]. In this study, the tissue damage in question is follicular atresia or follicle failure to develop [44]. The results of this study correspond to Li et al (2020): cigarette exposure causes follicle loss by inhibiting autophagy and pyroptosis activation [45].
Follicular damage means mitochondrial damage to granulosa cells, consequently triggering a sustained autophagy reaction and ending in granulosa cell death resulting in a reduced number of follicles [39]. A decrease in the number of primary, primordial, and de Graff follicles affects estrogen production and inhibits ovulation [46]. This is in accordance with the results of research by Kole et al (2020), cigarette smoke is known to cause a decrease in the number of follicles at all stages [24]. Wesselink et al 2019 found women smokers had low fecundity. Cigarettes were found to have no negative effects on IVF, as evidenced by the fertilization rate which was no different from non-smokers[29]. However, in the second offspring (F2), it was found that the rat cubs experienced a decrease in brain function [34].
The loss of ovum at all stages is a clear indication that exposure to cigarette toxicants alters the ovaries' cell structure. The decrease in ovum was brought about by the activation of pro-inflammatory cytokines and oxidative stress indicators by CS. This occurrence causes cell damage, particularly to the GCs that make up the ovaries, which impairs the ovaries' ability to secrete hormones.
Cigarette Smoke against Reproductive Hormones
Oxidative stress from cigarette smoke can result in impaired GnRH performance, resulting in failure of secretion and synthesis of FSH and LH [25]. When GnRH does not secrete FSH and LH, there is an inhibitory process in folliculogenesis that has an impact on decreasing estrogen production by suppressing 21 hydroxylaxes [47]. Estrogen is needed by the body for the ovulation process, where hormone levels will be normal if follicular development takes place normally [46]. Toxic substances in cigarette smoke will increase mRNA expression in VEGF which will modulate prostaglandins, as a result progesterone synthesis is inhibited and insufficiency occurs in the corpus luteum [48]. Corpus luteum insufficiency, also called luteal phase disorder, is a manifestation of ovarian failure where no follicles develop and eventually anovulation occurs. This condition can cause menstrual abnormalities [49].
Chen et al, (2022) found that there is a decrease in CYP19 which results in a decrease in estradiol synthesis and leads to hyperandrogenism and the formation of hemorrhagic cystic follicles [50]. Exposure to CS in the ovaries causes follicles to form abnormally and creates an imbalance in the hormones that leads to a decrease in the release of estrogen. Low estrogen causes LH to fall and FSH to stay at its highest. This has an impact on folliculogenesis later on. Therefore, reproductive diseases that are mutually exclusive arise from exposure to CS.
Cigarette Smoke against Oviduct
Rauf et al (2022) found an incidence of fallopian tube mucosa flattening after rats were injected with nicotine. His other research also found that nicotine injection can result in thinning of the wall thickness of the ampulla and isthmus, as well as the height of the epithelium of oviduct [23]. Smoking can increase inflammation, as seen with IL-6, TNF-α, and IL-8 which are increased [51]. Inflammation results in injury to cells that require self-repair mechanisms through proliferation [52]. Estrogen functions in the immune system of the oviduct mucosa by regulating S100A8, thereby inhibiting inflammation [53]. However, low estrogen levels due to nicotine exposure will inhibit cell proliferation which leads to cell loss and thinning of the isthmus layer [54]. Thinning of the smooth muscle layer of the fallopian tubes can decrease peristaltic movements that serve to help the movement of the ovum towards the uterus [55]. It is well known that exposure to toxins raises proinflammatory cytokines. One of the harmful effects of cigarette smoking is a drop in estrogen, which also causes inflammation, which in turn causes cell loss. Microscopic examination therefore reveals a weakening of the structural layer that constitutes the oviduct. These anomalies increase the chance of an ectopic pregnancy by preventing fertilization products from reaching the endometrium.
Cigarette Smoke against Uterus
There was a decrease in endometrial proliferation and an increase in cell death after CSE-induced (Cigarette Smoke Extract) above 1% and 0.025% CSE treatment resulted in an increase in VEGF through accumulation of factor-1α. CSE-induced oxidative stress plays a role in the release of VEGF [56]. Increased VEGF is an adaptive response to the presence of oxidative stress [57]. VEGF is essential for placentation and implantation, however when the amount is excessive, it can inhibit normal angiogenesis through over-stimulation of blood vessels and causing disruption of the structure of blood vessels [58]. CSE suppresses various regeneration functions in the endometrium, such as migration, self-repair, and pluripotency through SERPINB2 activation that can affect the implantation process [59]. Experimental animals exposed to e-cigarettes are known to have almost no embryo implantation sites despite the presence of high progesterone [60]. Angiogenesis and proliferation are highly impacted by the reduced estrogen brought on by CS, and this is where disruptions will arise. Endometrial thickness will decrease as a result of an increase in cell death (CD) in the endometrium after a reduction in proliferation. Following this thinning, there is a reduction in vascularization, which lowers the capacity of the conception products to be implanted.
Conclusion. The toxic effects of cigarette smoke are multifaceted, including ovotoxicants. Cigarette smoke affects female reproduction by increasing oxidative stress, triggering inflammation, increasing apoptosis to follicle loss and decreasing the synthesis of estrogen, GnRH, FSH, LH, progesterone, and estradiol. Smoking is known to damage the regulation of reproductive hormones that affect the disruption of reproductive function of the ovaries, uterus, and oviduct. Although it has no effect on IVF, smoking should still be avoided given its adverse effects on reproductive cells and hormonal balance. Therefore, it is expected that there will be a decrease in cigarette consumption patterns considering the adverse effects caused by reproduction.
Financial support
No financial support has been provided for this work.
Thanks
The author thanks the Master of Midwifery Programme, Faculty of Medicine, Brawijaya University, for access to literature





















Reference lists