The role of mental disorders in the pathogenesis of atopic dermatitis (review)
Abstract
Background: The problem of atopic dermatitis has received significant attention from researchers across different fields over the years. Despite its high prevalence, there remains an incomplete understanding of the underlying pathogenetic mechanisms, leading to ineffective therapeutic strategies. This lack of consensus regarding a unified model of dermatitis development creates challenges in selecting appropriate treatment options. The aim of the study:To analyze the current scientific literature data describing the relationship between central nervous system damage, psychogenic factors and the development of atopic dermatitis. Materials and methods: Data were searched in the electronic libraries of scientific articles PubMed, eLIBRARY.RU, and Google Scholar. A total of 41 publications corresponding to the objectives of the current review were analyzed. Results: Numerous studies highlight the dual contribution of exogenous (environmental) and endogenous (internal) factors in the etiology of atopic dermatitis. Psychogenic elements, particularly psychological stress, emerge as key drivers influencing disease progression. Recent advancements in psychoneuroimmunology underscore the profound effect of psychophysiological variables on immune responses. Additionally, a correlation exists between the degree of pathological changes, distribution of skin lesions, and the severity of associated psychopathological manifestations. However, these findings predominantly focus on adults, with less exploration into pediatric populations where mental health aspects are often overlooked. Current investigations typically prioritize cutaneous pathologies rather than considering broader implications related to systemic impacts. Conclusion: Further investigation into the interplay between psychogenic influences and individual personality traits could provide valuable insights into the mechanisms underpinning atopic dermatitis. Addressing the gaps in our knowledge concerning the contributions of intrinsic neurological anomalies and their consequences on autonomic-nervous and immunological balance may yield more effective diagnostic tools and therapies
Keywords: atopic dermatitis, mental disorders in atopic dermatitis, the mechanism of their occurrence, literature review
Introduction. Atopic dermatitis (AD) is the result of the impact of a large number of pathological factors on the human body, the mechanism of which has yet to be fully studied. Today, it is known that the pathogenesis of atopic dermatitis affects all human organ systems. Over the past 20 years, there has been an increase in the incidence of AD by more than 2 times. The prevalence of AD varies depending on the region [1, 2] and among the paediatric population exceeds the figure of 20%, and among the adult population it reaches almost 10% [3].
The incidence of atopic dermatitis (AD) among children in different regions of Russia ranges from 10 to 28%, accounting for 50–75% of all allergic diseases [3].
The role of genetic influence on the occurrence of AD is obvious. For instance, AD develops in 81% of children when both parents suffer from this disease, and in 56% of children when only one parent is ill. Moreover, the risk of developing AD increases 1.5 times if the mother is ill [3]. AD is a disease with a genetic predisposition [4, 5], which is strongly influenced by the innate and adaptive immune response as well as environmental factors [6, 7, 8].
Researchers attach great importance to psychogenic factors, primarily to psychological stress [9]. Modern advances in psychoneuroimmunology demonstrate an enormous influence of psychophysiological factors on the immune system. Psychotraumatic factors among women, intrafamilial stressors are in first place in terms of prevalence and significance (44.1%); among men, work-related stressors predominate (29.8%) and family problems are less frequent (24.8%). At the same time, 34% of the patients experienced the onset or recurrence of the skin disease 1-2 days after severe stress. Severe stressful situations account for 28% of all cases, psychic trauma of moderate severity occurs in 39% of cases. As a result of psychogenic exacerbation of atopic dermatitis, the production of regulatory neurotrophins and neuropeptides increases. This leads to impaired cytokine secretion and imbalance in cellular immunity, which in turn contributes to the development of inflammation [10].
Domestic scientists noting that the concentration of a neurotrophic factor in the blood closely correlates with the activity of the disease support the latter conclusion. In morphofunctional terms, the immune system is not isolated from the central nervous system but serves as the object of its regulatory influences.
Chronic stress is commonly associated with immunosuppression. The relationship between the most important systems of the body is carried out through endocrine factors. Another possible mechanism for the transformation of psychogenic effects during aggravation of AD is the involvement of neural pathways providing signal transmission between the central nervous system (CNS) and the skin. This conclusion was based on the identified features of clinical manifestations. Such as the symmetry of the rash, the complete absence of rashes in areas of skin denervation, the occurrence of erythema and itching when experiencing a stressful situation. Thus, it was established that with AD, a high density of nerve endings is observed in areas of chronic rashes.
The aim of the study. To analyze the current scientific literature data describing the relationship between central nervous system damage, psychogenic factors and the development of atopic dermatitis.
Materials and methods. Data were searched in the electronic libraries of scientific articles PubMed, eLIBRARY.RU, and Google Scholar. The search was conducted using the following keywords: atopic dermatitis, pathogenesis of atopic dermatitis, psychosomatic disorders, neuropsychiatric model. Initially, 183 publications were retrieved. Of these, 74 did not meet the inclusion criteria, 37 were duplicates and were therefore excluded, and 31 were of poor quality or lacked sufficient information. Ultimately, 41 original publications aligned with the aims of the review were analyzed.
Inclusion Criteria:
- Original research, qualitative reviews, and meta-analyses published from 2010 until today.
- Studies focusing on the interaction between mental disorders and atopic dermatitis, as well as the psychoneurological component in the pathogenesis of the disease.
- High levels of evidence (classification levels 1 and 2 according to the Oxford Centre for Evidence-Based Medicine scale).
- Statistically significant outcomes (p≤0.05).
- Accessible full text or sufficient information to evaluate the study comprehensively.
Exclusion Criteria:
- Unreliable or poorly executed studies.
- Papers not addressing the topic of the link between mental disorders and atopic dermatitis.
- Cases of duplicate publication (only the most complete version was retained).
- Small sample sizes (less than 50 subjects) unless the study had exceptional relevance or uniqueness.
- Partial texts or fragmented publications preventing a full assessment of methodology and results.
Theories on the occurrence of atopic dermatitis in children
The formation and course of AD in children is significantly influenced by genetic predisposition to allergic reactions with polygenic forms of inheritance. It should be noted that it is not the disease itself that is inherited, but a set of genetic factors that contribute to the formation of allergic pathology [11]. It has been established that, in most cases, atopic dermatitis is a hereditary condition. Studies show that 40% of patients have one or more family members with signs of atopic dermatitis in their anamnesis. It is generally accepted that the prevalence of AD among children whose parents suffer from AD is more than 60%. If both parents are ill, then AD develops in the child in more than 80% of cases. The researchers haven’t established differences in gender-based inheritance. According to Toppila-Salmi S. (2019), a predominant influence of the maternal line is assumed. For instance, a connection with atopic diseases on the mother’s side is detected in 60-70% of cases, less often on the father’s side – 18-22% of cases. AD is often combined with respiratory atopies [12].
Immune mechanisms of atopic dermatitis
Russian and European scientists have established that the main mechanism in the pathogenesis of AD is immune dysfunction [13]. In the pathogenesis of AD, two factors are crucial, namely impaired skin barrier function and violations of the body’s immunological reactivity, with a shift in the balance between Th1 and Th2 lymphocytes towards the latter, as well as an increase in the production of corresponding cytokines [14].
Normally, Th 1 and Th 2 immune cells act in a balanced manner. However, when AD is biased towards hyperactivation Th 2, which leads to an inadequate immune response and disruption of IgE production. A significant decrease in the level of gamma interferon is also noted. It could be argued that this mechanism plays a key role in the development of AD. It should be noted that in patients with atopy, the number of Langerhans cells, which are the main cells of the skin immune system responsible for the accumulation of IgE-mediated allergens in the skin and their presentation to T lymphocytes, is significantly higher than in healthy people [15].
The pathogenesis of AD is not limited to the reagin type of allergy by which, with increasing duration of the disease, there is a persistent imbalance between Th2 and Th22/Th1 and Th17, which remains even during the remission of dermatosis, as well as disturbances in the cytokine profile, in particular the IL-4/IL-13 ratio [16].
Dendritic cells activated by mediators of acute inflammation infiltrate the epidermis and initiate an immune response through the Th1 pathway, leading to increased production of INFγ, IL-2, IL-12. Skin brushing exacerbates damage to keratinocytes, mast cells and macrophages that contain IgE. This triggers the release of IL-1, TNF-α, platelet-activating factor, leukotrienes and other mediators that support the inflammatory process [15].
In the genesis of chronic inflammation in AD, we cannot exclude autoimmune processes and features of the immune response, which may contribute to the development of a hypersensitivity reaction and induce the proliferation of autoresponsive T cells. At the same time, the development and course of immune reactions in the skin is influenced by the peripheral nervous system [17].
The intensity of itching in patients with chronic dermatoses depends on the severity of cutaneous innervation by nerve C-fibers. AD may be only triggered by various environmental factors in people prone to it [7] Food sensitization is also of importance in the pathogenesis of AD. It is well known that when following a hypoallergenic diet and refusing to eat foods such as eggs, milk, seafood, mushrooms, cereals, legumes, citrus fruits, the severity of AD is alleviated, which is observed in more than 90% of patients with severe AD [8]. To date, it has been established that the causes of constant exacerbation of allergic reactions in children with AD are disorders (chronic diseases of the gastrointestinal tract), hepatobiliary system, parasitic invasions) and true food allergy [18]. In addition to the above-mentioned factors affecting the course of AD, the researchers point to the role of many background disorders in manifestation of the disease. In their opinion, these disorders may enhance certain components of pathogenesis: internal focal infections, dysmetabolic nephropathies, interstitial nephritis, disorders of intestinal biocinosis, congenital, genetically mediated intestinal fermentopathy, impaired metabolism of fatty acids in formed elements, blood plasma, and adipose tissue [19].
The role of CNS damage in the pathogenesis of atopic dermatitis
Great importance in the development of AD is given to the pathology of the central nervous system. Interesting results were obtained during the neurological examination of children with atopic dermatitis. A total of 124 children were examined. In 71.4% of cases, corresponding neurological symptoms were detected, which, according to the authors, indicated dysfunction of the brain at the level of the cortex and limbic-reticular complexes [20]. So, based on the results of a study conducted using cardiointervalography under the Reocard program, notes the secondary nature of changes in autonomic regulation that progress against the background of the torpid course of atopic syndrome. When examining the functional state of the central and autonomic nervous system (EEG, REG, ultrasound dopplerography of vessels in the brain and spinal cord), pathological changes were identified in 76.6% of AD patients. Only a few publications in modern literature are devoted to the study of EEG in AD. The study was carried out exclusively by Russian authors. EEG is a prognostic examination method, since persistent EEG changes after treatment indicate the possibility of a relapse in the near future in some patients. EEG examinations in children and adolescents with skin pathology showed the signs of residual organic cerebral insufficiency in all patients.
Of particular interest is an EEG examination of children with AD conducted on a "Neurocartograph" computer encephalograph using color mapping, spectral and correlation analysis. In 36% of the children, the absence of alpha rhythm on the EEG was revealed, which, according to the authors, is due to profound changes in the functional state of the cerebral cortex and subcortical structures [20]. The revealed changes in the cerebral bioelectrical activity usually manifested themselves as disturbances in the regularity of the basic rhythm, the inequalities of its frequency and amplitude, disturbances in zonal differences, the presence of slow waves, mainly in the Ɵ-band, sometimes in the form of bilaterally synchronous bursts, single acute oscillations, and impaired reactivity. As a result, three variants of changes were presented on the EEG with an increasing degree of severity (phasing) of disturbances in the cerebral bioelectrical activity (Table 1).
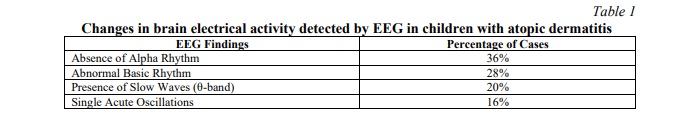
These EEG findings illustrate disrupted electrical functioning in the brain, consistent with profound changes in cortical and subcortical areas. Three distinct phases of EEG disturbance severity were documented, emphasizing the dynamic nature of neurological perturbations in AD.
Rheoencephalography in almost all examined AD children enabled establishing the asymmetry of blood flow with changes (increase or decrease, often combined) in blood filling and tone of medium- and small-caliber vessels of anterior and vertebral artery circulation as well as the difficulty in venous blood flow. By means of REG, in AD patients, a dystonic state of the vessels in posterior circulation with asymmetry of blood flow up to 50% and a tendency of the cerebral vessels to hypertonicity was determined. The authors linked the formation of dermatosis clinical forms with the influence of certain risk factors in the corresponding age periods. Thus, both external (physical, chemical, biological) and internal (pathology of the nervous system, gastrointestinal tract, genetic predisposition and immune disorders) factors have a direct impact on the occurrence and development of atopic dermatitis [20].
The role of psychogenic and personal factors in the development of atopic dermatitis
The provocative role of psychogenic factors in the development of skin diseases was noted by many physicians [21]. At the end of the 19th century, Brocq L, Jacquet L. introduced the term “psychoneurodermatitis”, which, according to the researchers of that time, clearly indicated the origin of the disease.
The direct impact of stress factors on the course of AD is based on the activation of the hypothalamic-pituitary-adrenal system, which is responsible for the transmission of control impulses from the central nervous system to the immune, endocrine and other systems. In atopic dermatitis under conditions of stress there is a decrease in the reactivity of the hypothalamic-pituitary-adrenal system. The described mechanisms contribute to the exacerbation and development of atopic process under the influence of psychogenic factors. For instance, researchers revealed a statistically significant increase in the number of CD8+ lymphocytes and CLA in the blood, expressed by more than 80% of T cells infiltrating the skin [21]. It is well known that in atopic dermatitis, CLA causes an increase in IL-13 and IL-5 levels. Excessive blood levels of CLA cells as a result of stress indicate an increased ability of T lymphocytes to migrate into eczematous damaged skin during psychological stress, reflecting a link between psychoneuroendocrine mechanisms and Alzheimer's disease [21].
Another most probable mechanism of stress effect on skin condition is the influence of neuropeptides and their receptors on the transmission between the central nervous system, skin cells and the immune system. The described mechanisms are reflected in the concept of neurogenic inflammation in AD.
It should be noted that for more than half a century, studies have been conducted to establish the role of personality traits of the patient in the development of AD. To date, no personality type specific to AD has been identified [22]. However, personality characteristics common to patients with AD have been established. Among them are mood swings, irritability, anxiety, depression, and neuroticism [23]. It should be noted that AD patients are characterized by the whole spectrum of nosogenic reactions complicating the course of the disease. The most important factor is the recurrent nature of the disease, subjective intolerance of itching, resistance to therapy, as well as cosmetic defects of the skin at the site of rashes [3]. In other words, the skin symptoms themselves are provoking factors and have a psychotraumatizing effect. They contribute to the progression of the disease in the form of the formation of new waves of exacerbations "inside" the relapse. The result is a kind of "vicious circle" of the disease [9]. Thus, we can speak about a close relationship between mental disorders and the course of clinical symptoms of skin diseases [24].
AD patients are characterized by certain neurotic personality traits. These include alienation, mood swings, depression, tension, aggressiveness, anxiety, and hypochondria. In turn, the reaction of introverted individuals, expressing anxiety and “hostile emotional conflict,” often manifests itself in the form of scratching the skin [25].
The psychological portrait of a patient with atopic dermatitis is reflected in many literary data. Most often, the characteristics of such patients include anxious-depressive features, pronounced tension, which is largely due to the disease itself with its frequent exacerbations, discomfort in the form of itching and disfiguring lesions of the skin [26]. Numerous studies have also demonstrated an association between certain subtypes of depression and elevated levels of systemic inflammatory markers, such as interleukin-6 (IL-6) and C-reactive protein. Elevated levels of these biomarkers in AD patients may indicate a general inflammatory aetiology [10].
Skin lesions, their prevalence and severity of symptoms are closely related to the development of psychopathological changes in the patient. It is noteworthy that the duration of the skin disease (eczema, psoriasis, atopic dermatitis) does not affect the spectrum of concomitant mental disorders, in contrast to the localization of the pathological process, which is of great importance [22].
Today, there is no doubt that it is important to study the mechanisms of mutual influence of psychogenic and personal risk factors of the patient on the development and exacerbation of the atopic process. It is obvious that the relationship between psychological, personal and physiological components of the pathogenesis of atopic dermatitis allows us to classify this disease as a psychosomatic disorder.
Impact of positive emotions and non-pharmacological approaches on the course of atopic dermatitis
Multiple scientific studies have demonstrated the beneficial effects of laughter, with researchers from various countries conducting experiments measuring its physiological impacts and advantages. It's been established that laughter helps reduce the production of allergen-specific IgE antibodies, diminishing allergic skin reactions and significantly boosting the activity of natural killer cells. Positive emotions consequently exert a noticeable influence on both hormonal and immune responses [27].
Certain studies have shown that kissing can substantially alleviate skin conditions associated with allergies by reducing levels of neurotrophic growth factors such as NGF, BDNF, NT-3, and NT-4 in patients with atopic dermatitis. These findings imply that kissing plays a significant role in neuroimmunological studies concerning atopic dermatitis [28].
Music offers yet another advantage, helping divert patients’ attention away from distressing experiences or negative thoughts, greatly enhancing their quality of life. In addition, musical accompaniment can have a regulatory effect on immune responses, resulting in an increase in the number of lymphocytes, T cells, CD4 + T cells and memory T cells, as well as an increase in the level of IFN - γ and IL -6. These changes directly affect the barrier function of the skin and the severity of general symptoms of atopic dermatitis.
Contemporary research suggests incorporating familiar and enjoyable music into routine music therapy sessions to help mitigate symptoms of multiple illnesses, including atopic dermatitis [28].
Additionally, a notable correlation has emerged between the progression of atopic dermatitis and watching entertaining television programs. Observations show that watching movies causes measurable shifts in blood parameters, mitigating allergic responses. Specifically, the count of plasma neutrophils noticeably drops after film viewings, thus improving indirectly mediated allergic reactions [29].
Emphasizing well-being, humor, and joy as potential therapeutic interventions, it's vital to incorporate positive emotions into treatment regimens for patients with atopic dermatitis.
Mental disorders in atopic dermatitis
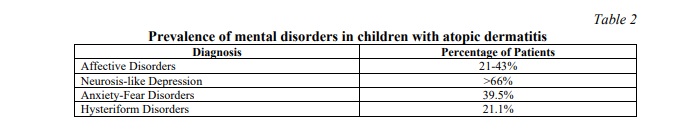
It's known that psychological disorders, including depression and anxiety, are closely connected to the development of atopic dermatitis and demand thorough attention [30]. Data indicates that mental disorders are prevalent in a sizable portion of patients with atopic dermatitis (Table 2), with nonpsychotic mental disorders occurring in nearly half of young patients afflicted by this condition. Remarkably, in severe cases, roughly two-thirds of patients encounter a variety of psychological issues, spanning from anxiety and phobia to depressive symptoms [31].
It was found that children with atopic dermatitis are more likely to have depressive and anxiety disorders, behavioral disorders, autism spectrum disorders and hyperactivity disorder. They are characterized by suicidal thoughts and suicidal tendencies compared to healthy peers [23]. Concurrently, atopic dermatitis frequently contributes to sleep disturbances, lowered self-esteem, and social difficulties in peer relationships [32].
Most authors note the severity of depressive disorders, which correlate with the severity of skin manifestations [10]. Depressive reactions were predominant, cyclothymia was more typical for common forms of AD (28.7%). AD patients were characterized by anxious (39.5%) and hysterical (21.1%) variants of neurotic development.
It was found that in the younger age group (12-13 years old), mental disorders manifested themselves in the form of short-term neurotic reactions and behavioral disorders. In the middle age group (14-15 years old), mental disorders were characterized by greater severity and clinical polymorphism with emotional experiences of the disease, especially a cosmetic defect. In the senior group (16-17 years old), persistent and clinical mental disorders as well as disorders that fitted within the framework of pathocharacterological development of personality were more often observed [33, 34]. The researchers have an ambiguous opinion regarding the relationship between depression, pain, itching and tingling. An interesting position is taken by other researchers who claim that sensations of the skin (burning, pain, etc.), having an obvious organic genesis, which can be regarded as equivalent to the latent course of depression [35, 36, 37]. It is also known that depression occurs with changes in a number of immunological indicators [38].
At the neuroendocrinological level, a number of signs common to depression and AD have also been found.
Today, the study of the prevalence and severity of anxiety and depression in patients with atopic dermatitis is conducted mainly by dermatologists using appropriate psychometric scales [39, 40].
It is generally accepted to attribute atopic dermatitis to a group of psychosomatic disorders characterized by variability of symptoms. Some experts contend, however, that only a fraction of cases fit this categorization, as many patients follow an autonomous disease trajectory. Meanwhile, the efficacy of treatments for atopic dermatitis and the length of remission periods tend to decline notably [41].
Conclusion. Atopic dermatitis is a complex disease involving immune, genetic, and psychoneuroimmunological factors. Comorbid mental disorders, such as anxiety and depression, exacerbate symptom severity and flare-ups. Effective treatment requires an interdisciplinary approach integrating dermatological, psychopharmacological, and psychotherapeutic measures to break the vicious cycle of psychosomatic interactions and improve long-term outcomes.
Financial support
No financial support has been provided for this work.





















Reference lists