Gastrointestinal stromal tumors in elderly patients
Abstract
Background: Gastrointestinal stromal tumors (GISTs) account for 1 to 3% of all primary malignant tumors of the gastrointestinal tract. The global incidence of GISTs varies in the range of 7-15 cases per 1 million people per year. In about 95% of cases, the incidence is sporadic. Despite the fact that some success has been achieved in the treatment of this pathology, the problem of GISTs treatment is urgent, especially in elderly and senile patients in particular. The aim of the study: To study the age-related characteristics of GISTs development in patients of older age groups. Materials and methods: A retrospective analysis of 56 clinical cases of GISTs in patients of different age groups according to the WHO classification was carried out in the study. Results: The most common variant of the immunohistochemical structure was the spindle cell one – 62.5%. In most cases, tumors were localized in the stomach – 82.2%. Elderly patients had larger tumor sizes compared with young and middle-aged patients. In patients of older age groups, the disease was most often detected at stage II. In most cases, a comorbid pathology was detected, most often a combination of several diseases of the cardiovascular system. Conclusion: In patients of older age groups, the spindle cell structure of the GISTs is most common, the tumor was most often localized in the stomach (77.4%), most often the tumor was localized along the lesser curvature. In most cases, the tumor was up to 10.0 cm in diameter. On average, the disease was detected at stage II. Comorbid pathology occurred in 87.3% of cases. In 2020-2021, the disease was detected more often, the of tumors sizes were smaller, due to an increase in the number of CT scans of the chest for the diagnosis of the new coronavirus infection.
Keywords: GISTs, cells of Cajal, elderly patients, oncologic pathology, immunohistochemical structure, mitotic index
Introduction. Gastrointestinal stromal tumors (GISTs) are the most common mesenchymal tumors in the gastrointestinal tract (GIT). These types of tumors account for 1 to 3% of all primary malignant tumors of the gastrointestinal tract [1]. For the first time, GISTs were described in 1980 as tumors originating from the stomach smooth muscles, after the introduction of immunohistochemical and molecular diagnostic methods, this type of neoplasm was isolated into a separate group [2, 3].
Currently, in most cases the molecular and biological mechanisms of the gastrointestinal stromal tumors occurrence are associated with a mutation of the KIT gene and, to a lesser extent, PDGFRA, encoding proteins of transmembrane receptors of stem cell growth factors (CD117). These tumors originate from interstitial cells of Cajal involved in the control of spontaneous gastrointestinal motility by generating slow electrical waves. Thus KIT is highly expressed not only in the cells of Cajal, but also in hematopoietic stem cells, melanocytes, mast cells [4, 5].
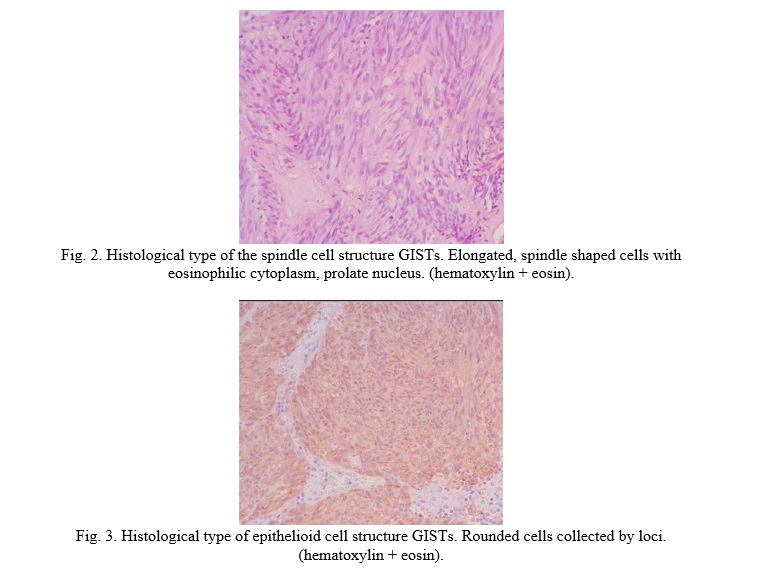
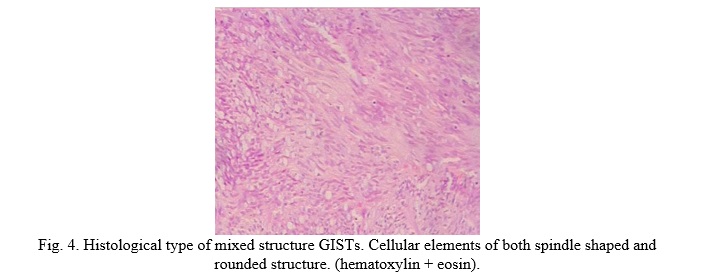
Histologically, GISTs are usually presented in the form of sharply demarcated, submucous or subserous tumors, with the following types of cytomorphology: 1) spindle-shaped (70%); 2) epithelioid (20%); 3) mixed [6]. According to some authors, the global incidence of GISTs varies in the range of 7-15 cases per 1 million people per year. There are regional fluctuations in the incidence, so in Western countries the incidence is 10-15 cases per million people per year, in Asian countries the incidence is the highest making 16-20 cases per million people per year [7, 8]. As a rule, the disease is sporadic, only about 5% of GISTs are included in such genetic syndromes as: Carney-Stratakis syndrome; Carney’s Triad; Neurofibromatosis type 1 (NF1); Primary familial GISTs syndrome [9, 10].
However, by histological, phenotypical and immunomorphological features, sporadic cases of GISTs and cases of the above syndromes do not differ [11]. Most often, metastases are localized in the liver (65%), peritoneum (21%), rare localizations of metastases include bones, lungs, lymph nodes. These tumors can be localized in any part of the digestive tract, however, most often GISTs are found in the stomach (about 60%), small intestine (20-30%), rarely in the omentum and mesentery, localization outside the intestinal tract is the least likely, and originates from the cells of Cajal randomly scattered on the peritoneum and its derivatives during embryogenesis [12, 13].
The incidence of the disease in men and women is approximately the same. There is an age-related heterogeneity of the disease, for example, young and middle-aged people suffer from it much less often, patients of older age groups are prone to the disease more often. So, the peak incidence is at the age of 50-70 years old [14]. The main treatment method for GISTs is surgery. Medium and low risk tumors do not require adjuvant therapy, while high risk GISTs are supplemented with Imatinib in addition to surgical treatment. However, Heinrich M.C. et al. in their study described the mechanisms of secondary tumor resistance to Imatinib and showed the efficacy of Sunitinib as a second-line therapy [15, 16]. There is currently a third-line drug – Regorafenib. However, the treatment of metastatic forms of tumors with multiple heterogeneous mutations and resistant subclones remains an urgent problem [17]. As for the survival rate of patients with GISTs, there are the following gradations of 5-year survival: in case of localized forms of the disease, 5-year survival can be expected in 93% of patients, in case of the locally spread process – 80%, in patients with GISTs with metastases the 5-year survival rate is 55% [18].
Thus, GISTs are tumors of mesenchymal origin, predominantly of a sporadic nature, less often as part of genetic syndromes. Diagnosis is based on an immunohistochemical examination of the removed tumor. The main method of treatment is surgical, however, in case of unfavorable prognostic factors, it is supplemented with targeted therapy. Further studies of this pathology, as expected, will be aimed at defining tumor subgroups and selecting the optimal combinations of various therapies, as well as long-term adjuvant therapy. Given that the peak incidence occurs at the age of 60-70 years old, GIST is an urgent gerontological problem. There are practically no age-related GISTs studies.
The aim of the study. To study the features of GISTs in patients of older age groups, to carry out a comparative analysis including patients of young and middle age.
Materials and methods. The study subject included 56 patients aged 32 to 85 years who were treated at the abdominal oncological department of the Kursk Oncology Scientific and Clinical Center (Kursk) from 2015 to the third quarter of 2021 inclusive with a diagnosis of gastrointestinal stromal tumor (GISTs). The average age of the patients was 68.78±2.52 years. The average weight of patients was 71.59±2.45 kg, BMI –27.8±0.79 (from 20.04 to 40.57).
The research material – medical records of inpatients. Red blood cell counts (erythrocyte concentrations and hemoglobin levels), leukocyte counts, basic biochemical blood counts (bilirubin, urea, creatinine, and total protein levels), tumor size, body mass index (BMI), comorbidity, tumor localization, immunohistochemical types of structure were analyzed in all patients, as well as the structure of disease detection (complaints, accidental detection, etc.) and the index of proliferative activity (Ki67).
The patients inclusion criteria for the study: immunohistochemically confirmed gastrointestinal stromal tumor, differentiated tumor structure (spindle cell, epithelioid cell, mixed), specified mitotic index and proliferative activity index (Ki67), localized tumor process, surgery, absence of other proven malignant process or radical treatment of neoplasms of any localization (patients with clinical group III) for 5 years or more, no metastases, no lethal outcomes during the period of hospitalization.
The analysis of the total sample was carried out in the first part of the study. A comparative age analysis of two groups of patients was performed in the second part of the study. For that purpose, the patients were divided, according to the WHO age classification, into two groups: the 1st group (control) – young and middle-aged patients (18-44 and 45-59 years old, respectively) – included 25 patients in it (44.6%); the 2nd group (main) – patients of older age groups (elderly and senile age (60-74 and 75-89 years old, respectively), this group included 31 patients (55.4% of the total sample).
For statistical analysis the data were grouped and presented in the form of tables. The patterns were revealed using correlation analysis of the obtained data with subsequent drawing of graphs and diagrams. The average value of the quantitative indicator (M), standard deviation (m), Student's t-test (t), the Pearson correlation coefficient (r) were calculated for statistical analysis of the obtained results validity. Statistical calculations were performed using computer software Microsoft Excel-2019 and Statistica 10. The significance of differences in the studied groups was assessed by the Student's t-test. The Pearson coefficient was used to determine the correlation between the studied parameters. In all cases, differences with the level of statistical significance p<0.05 were recognized as valid (statistical data analysis methods).
Results and Discussion
Analysis of the total sample
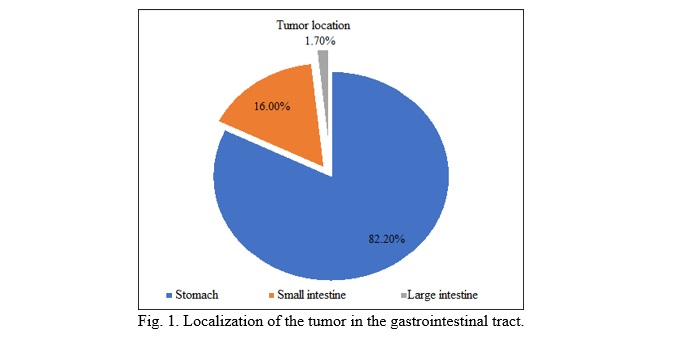
The distribution by gender in the total sample was as follows: 32.1% (18 patients) men, 67.9% (38 patients) women. In most cases that met the inclusion criteria, tumors were localized in the stomach – 82.2% (46 cases observed), in 16.0% of the cases (9 patients) – in the small intestine and in 1.7% of the cases – in the colon (ascending colon) (Fig. 1). The data obtained are consistent with the studies of Joensuu H. et al., who indicated that in most cases it is the stomach that is affected.
Based on the surgery protocol, we analyzed the lesion of the stomach depending on the part, and in most cases the lesser curvature of the stomach was affected – 45.6%, then the greater curvature – 39.1%, most rarely the posterior wall – 15.2% (7 cases). The most frequent lesion of the stomach, and in particular the lesser curvature, is quite explainable by the largest muscle mass, as well as the richest blood supply to the stomach and especially to the lesser curvature. (Fig. 2-4).
GIST, as a rule, have a rounded shape, with both intramural and subserosal location on a wide or narrow base. The largest tumor size in the studied sample was 24.0 x 22.1 cm, the smallest was 2.0 x 1.7 cm (detected by accident during EGD). The average tumor size was 883.8±7.76 cm (transverse size) by 67.43±5.61 cm (longitudinal size). In accordance with their size, the tumors most often had a T3 criterion (tumors between 5 cm and 10 cm in the largest dimension) according to the TNM classification 8th edition. Depending on the mitotic index, tumors are divided into two subgroups – those with a high and low mitotic index. A low mitotic index – less than 5% – was observed in 64.5% of the analyzed samples, a high mitotic index of 5% and higher was observed in 35.5% of the cases. A distinctive feature of GISTs staging is the combination of TNM and mitotic index. So, in most cases (55.8%) the disease was detected at stage I of the neoplastic process, at stage II – in 17.7% of the cases, and at stage III – in 26.5% of the cases.
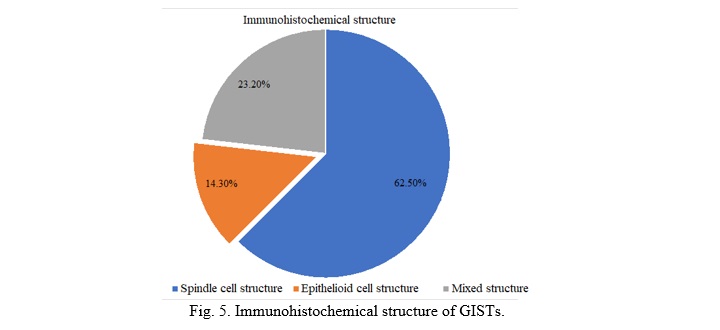
Most often – in 62.5% of the cases (32 patients) – tumors had a spindle cell immunohistochemical phenotype, a mixed structure was in 23.2% of the cases (13 patients), the most rare was the epithelioid cell type of the immunohistochemical structure – 14.3% of the cases (8 patients) (Fig. 5). The obtained data are consistent with the studies of Fülöp E. et al., establishing that the most common type of the immunohistochemical structure is the spindle cell.
Due to the fact that the main method for GISTs treatment is surgical, open surgery (laparotomy) was performed in 72.2% of operations, and 27.8% of the operations were performed laparoscopically. The percentage of laparoscopic surgical interventions has been steadily growing every year (Fig. 6-9). The trend has been most clearly observed since 2018-2019.
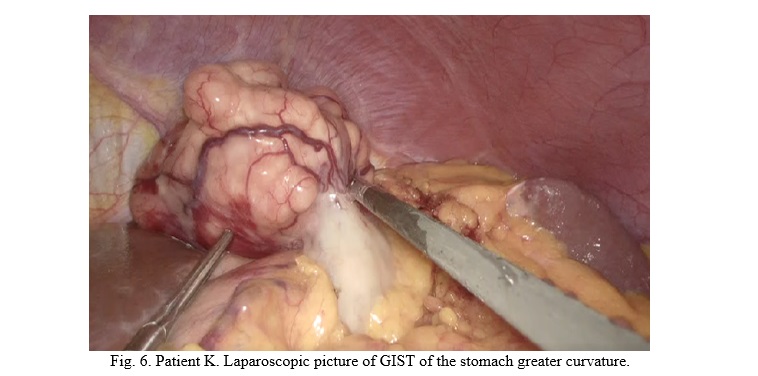
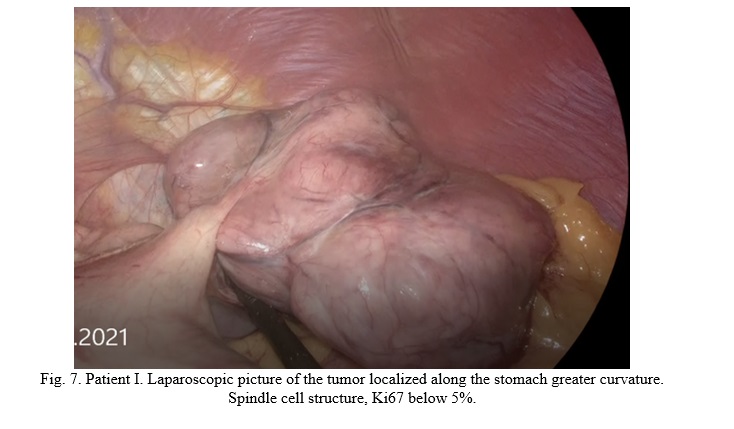
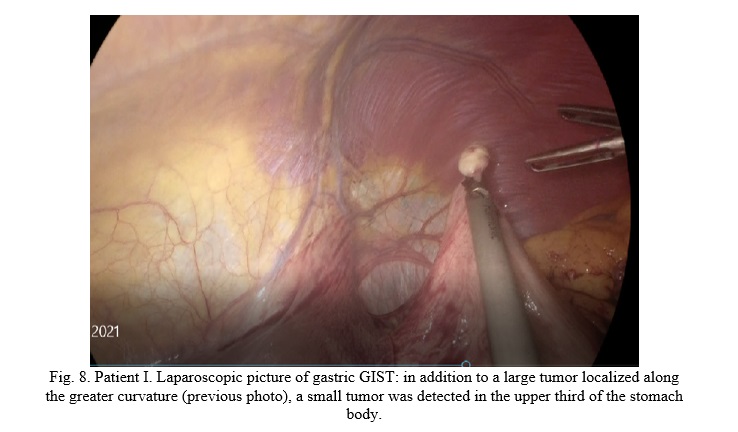

The abundant blood supply to the tumor, predominantly extraorganic location, uneven, bumpy contour, a capsule covering the tumor, a clear boundary between the stomach wall and the tumor are clearly visible. Due to the abundant blood supply, the tumor, quite often, manifests itself with gastric / intestinal bleeding. The choice of surgical aid was based on the following criteria: 1. The general condition of the patient (in particular, concomitant pathology); 2. The localization of the tumor – the possibility of radical surgical removal obtaining R0 of the resection margins (in some cases, the tumor had an oval shape and a large length, complicating the course of laparoscopic surgery); 3. The size of the tumor (in some cases, the tumors were large and the laparoscopic approach increased the operation time without improving the results). In each case, there was an individual and differentiated approach to the choice of surgery method. The average number of inpatient days in the studied sample was 14.8±0.99, the longest – 26, the shortest – 9.
At discharge, the hemoglobin level was 124.4±3.46 g/l, the level of erythrocytes was 4.0±0.11 x 1012/l, and the level of leukocytes was 7.6±0.39 x 109/l. Thus, the red blood counts were at the lower limit of the norm, the white blood counts were within the normal range. Biochemical analysis indicators at discharge were as follows: total protein level – 62.53±1.28 g/l, nitrogen metabolism – creatinine – 95.63±4.04 µmol/l; urea – 4.45±0.31, the bilirubin level – 10.95±1.01 μmol/l. There was a slight decrease in total protein level.
A positive correlation was found between age and tumor size (r = 0.51), so the older the patient was, the larger the tumor was. Accordingly, this correlation was observed between age and the disease stage (r = 0.58). Also, expectedly, there was a positive moderate correlation between age and total protein (r = 0.66), this feature indirectly reflects the syndrome of frailty and sarcopenia, aggravated by the oncological process and surgical trauma. A relationship was found between the age of patients and the level of creatinine (r = 0.65), age-related features of the urinary system, ultimately lead to a decrease in the level of filtration, nephrosclerosis, renal failure of varying severity. There was no convincing correlation between weight, BMI and the rest of the studied parameters. The obtained data are consistent with the studies of Gopie P. et al. [9].
Correlation was observed between the immunohistochemical structure of the tumor and localization depending on the stomach section (r=0.53), so the spindle cell type of the structure was most often localized along the stomach lesser curvature. It was also revealed that the advanced stage of the disease was associated (r=0.47) with a mixed variant of the tumor structure. No correlation was found between the localization of the tumor, depending on the stomach, and the size.
Despite the fact that the mitotic index is included in the staging parameters, the main parameter is the size of the tumor (T), which is why, quite naturally, a strong positive correlation (r=0.76) was found between the size of the tumor and the stage. No correlation was found between the stage of the disease and laboratory parameters at discharge, which suggests that GISTs do not cause severe anemia, hypoalbuminemia typical for adenocarcinomas. And, as a rule, most often they manifest either in gastric bleeding or a prolonged growing feeling of heaviness in the epigastrium.
The number of inpatient days depended on the method of surgery (r=0.56), so the more extensive the intervention was (for example: open proximal gastrectomy, elderly patient, with moderate anemia), the more inpatient days (24) patients spent in the hospital. There was also a correlation between the surgical method and the postoperative concentration of erythrocytes and the level of hemoglobin (r=0.64), so the laparoscopic method is, naturally, associated with less blood loss. No correlation was found between the surgery method, the number of inpatient days with other laboratory parameters.
Concomitant diseases in the total sample were detected in 86.1% of patients. Diseases of the cardiovascular system prevailed in the structure of concomitant pathologies. Diseases of the cardiovascular system of varying severity were detected in 83.2% of cases. Pathologies of the musculoskeletal system were detected (deforming osteoarthritis of varying severity, kyphoscoliosis) in 34.2% of cases. Pathologies of the endocrine system (diabetes mellitus) were revealed in 12.3% of cases. A comorbid pathology was observed in 44.5% of cases, and in most cases it was a combination of several diseases of the cardiovascular system (hypertension and calcification of the valvular apparatus of the heart with development of valve insufficiency of varying severity or hypertension and ischemic heart disease (IHD) – such combination of concomitant diseases was observed in 74.3% of cases, a combination of cardiovascular pathologies and diabetes mellitus were observed in all cases of endocrine system pathologies.
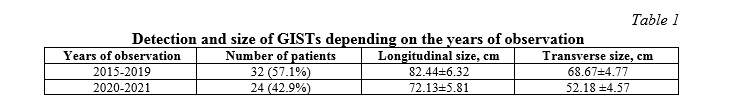
In the course of the study, the identified diseases were analyzed. Thus 32 cases of GISTs were detected (8-9 cases per year) in the period from 2015 to 2019 inclusively, as a rule, they were associated with chief complaints (bleeding, heaviness, discomfort, pain in the epigastric and/or umbilical region), less often associated with dynamic observation for various diseases (for example: follow-up examination after resection of breast cancer), while in the period from 2020 to the 3rd quarter of 2021, 24 cases were detected (10 in 2020 and 14 in the 3rd quarter of 2021). Analysis of GISTs detection in patients between 2020 to 2021 adds a new way of diagnosis – detected in the result of chest computerized tomography upon self-referral or dynamic monitoring of community-acquired pneumonia (Fig. 10, 11).
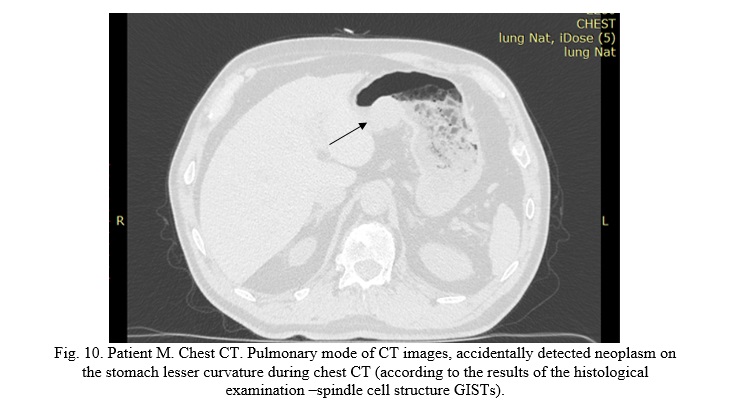
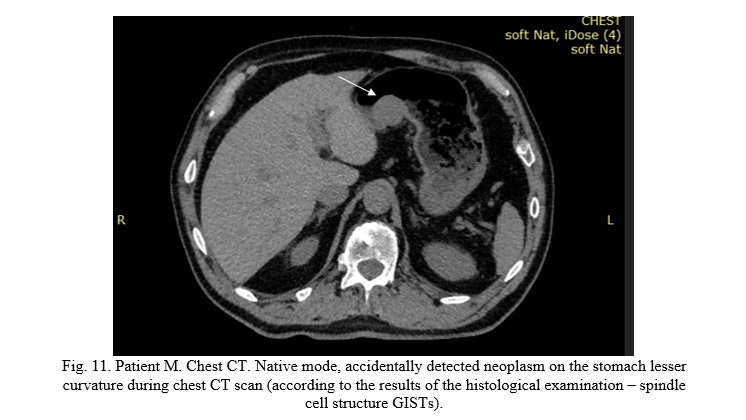
GISTs detected between 2015 and 2019 inclusively, were significantly (p=0.03) larger (mean sizes were longitudinal – 82.44±6.32 cm, transverse – 68.67±4.77 cm), while the sizes of tumors detected in 2020 and the 3rd quarter of 2021 were: longitudinal – 72.13±5.81, transverse – 52.18±4.57 cm. Therefore, expectedly, in 2020 and 2021 the disease was detected at the less advanced stages (Table 1).
As a rule, when performing a chest CT scan, the upper part of the abdominal cavity includes the scanned area, and then, patients are referred to an oncologist by CT diagnostics specialists.
Thus, a large number of CT examinations associated with the coronavirus infection pandemic increased the detection of GISTs and tumors at earlier stages before the development of clinical manifestations of the disease.
Comparative analysis of middle-aged patients and patients of older age groups
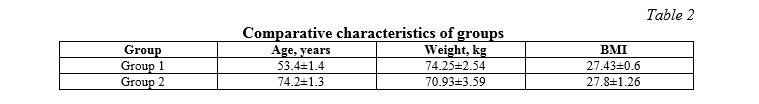
The age of young and middle-aged patients (group I) was 53.4±1.4 years, elderly and senile patients (group II) were 74.2±1.3 years old. There were no statistically significant differences in weight and BMI, the weight of patients in group I was 74.3±2.5 kg, in group II – 70.9±3.6 kg. Women accounted for 67.9% of cases (38 patients), men – for 32.1% (18 patients) (Table 2).
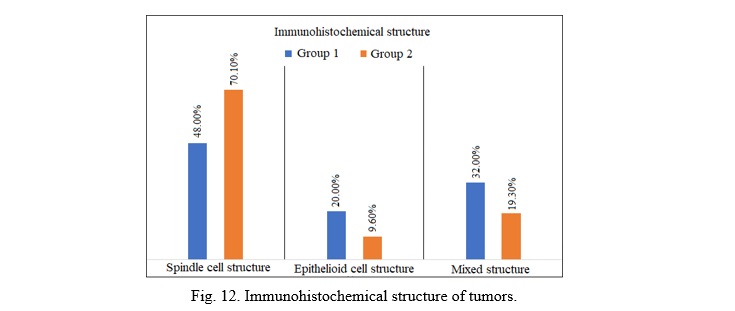
Statistically significant differences were obtained in the subtypes of the immunohistochemical structure of tumors between the studied groups. So, the most common type of the tumor structure in patients of older age groups was the spindle cell, which was found in 70.1% of cases, while in the 1st group this type of structure was found in 48% of cases (p = 0.043). The epithelioid cell type of the tumor structure was found in 20.0% of the patients of the 1st group and in 9.6% of patients of the 2nd group, the mixed type of structure was found in patients of young and middle age 1.7 times more often than in of elderly and senile patients (32.0% and 19.2%, respectively), p = 0.037 (Fig. 12).
It was also reliably established that the mitotic index was higher in patients of the 2nd group (p = 0.024). Thus, elderly and senile patients are expected to have a higher risk of aggressive tumor, requiring targeted therapy.
In both groups, the tumor was most often localized in the stomach. There were differences in the location of GISTs in the stomach sections, it was found that in patients of the 1st group, the tumor was most often localized in the greater curvature area – 36.0%, while in patients of the 2nd group the tumor was localized on lesser curvature in 41.9% (p = 0.004) of cases. Most likely, the tumor localization (lesser curvature) is associated with a more abundant blood supply and a larger muscle mass (Fig. 13).
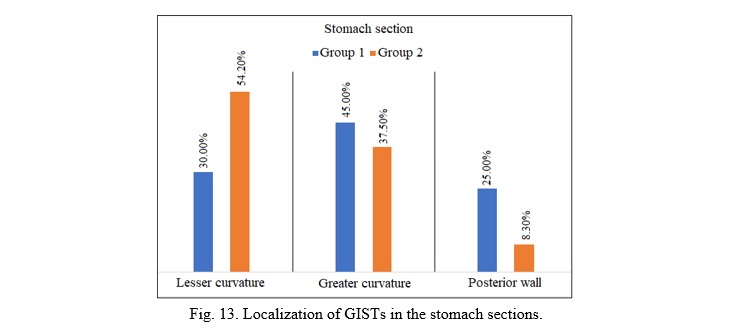
Localization of the tumor is important when choosing the method of surgical intervention, since it is technically the easiest to perform laparoscopic partial resection of the stomach in case of the localized form of the tumor process, and the most difficult when the tumor is located along the lesser curvature with the left gastric vessels involved.
In patients of the 2nd group the tumor sizes (86.33±14.58x72.8±12.27) were significantly (p=0.047) larger than in patients of the 1st group (68.5±7.99x43.63±5.77). Considering the higher mitotic index, large tumor sizes, it is natural that a more advanced stage (most often II) of the disease (p=0.016) was observed among elderly and senile patients.
There were no statistically significant differences in the methods of surgical treatment (open surgery or laparoscopic), as well as in the number of inpatient days.
A higher postoperative level of erythrocytes and hemoglobin concentration, expectedly, were observed in middle-aged patients 128.13±2.24 g/l and 4.14±0.09x1012/l, respectively, the same indicators in elderly and senile patients were 122.4±5.24 g/l and 4.0±0.16x1012/l. The level of leukocytes was also higher in young and middle-aged patients, which indicates a higher responsiveness, and its decrease in older and senile age (Table 3).
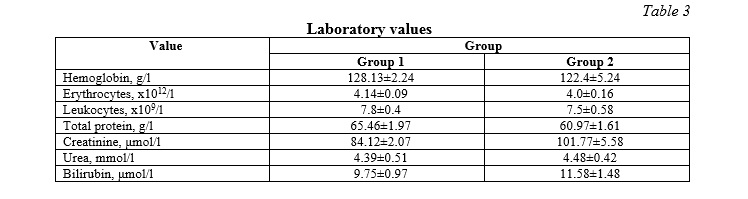
In the structure of concomitant pathologies, diseases of the cardiovascular system, of varying severity, prevailed in both groups, then endocrinopathies (diabetes mellitus). In the 2nd group, concomitant diseases occurred reliably (p=0.011) 2.3 times more often than in patients of the 1st group (Table 4).
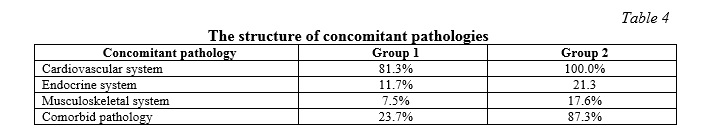
All elderly and senile patients had a concomitant pathology of the cardiovascular system (hypertension, coronary artery disease, heart valve stenosis, heart valve insufficiency, atrial fibrillation, lower limb varicose veins, post-thrombophlebitis disease, pulmonary embolism in medical background), comorbid pathology occurred in 87.3% of cases, and in 73.8% of cases several diseases of the cardiovascular system were observed, in some cases there were 3 or more diseases, in 17.6% – diseases of the cardiovascular system and musculoskeletal system, in 21.3% – diseases of the cardiovascular system and diabetes mellitus. In the 1st group, concomitant diseases were less common – in 65.7% of cases, mainly those were also diseases of the cardiovascular system (81.3% of cases), diseases of the endocrine system (11.7% of cases), diseases of the musculoskeletal system – 7.5% of cases. Comorbid pathology was much less common – 23.7% of cases (p = 0.003).
Thus, typically, the tumor was up to 10.0 cm in diameter based on the mitotic index and Ki67 had intermediate or high risk of aggressive behavior. On average, the disease was detected at stage II. The percentage of laparoscopic surgeries over the past 2-4 years, is steadily increasing and is replacing open surgeries. The obtained data are consistent with the studies of Miettinen M. et al. [1].
Diseases of the cardiovascular system were revealed in the structure of concomitant diseases in all elderly and senile patients, comorbid pathology was found in 87.3% of cases. Due to the increased frequency of chest CT scans, the frequency of tumor detection has increased, and the size of the tumors detected has become smaller.
The spindle cell structure of GISTs was most often found in patients of older age groups, the tumor was most often located in the stomach most often the tumor was located along the lesser curvature. The obtained data are consistent with the studies of Joensuu H. et al. [17].
A slight decrease in erythrocyte and hemoglobin counts was observed in older patients at discharge, the level of leukocytes was within the normal range. Total protein values were lower due to frailty syndrome, and creatinine and urea levels, on the contrary, were higher due to the age-related decline in renal function.
Conclusion. Thus, the study has newly revealed that patients of older age groups in most cases (77.4%) have spindle cell tumors, as a rule localized along the lesser curvature of the stomach. The tumors were detected at stage II and were less than 10.0 cm in diameter.
Comorbid pathologies (a combination of the cardiovascular system pathology with other diseases) were most common (87.3%) among patients of older age groups. There is a clear trend towards using the laparoscopic approach while performing surgical interventions. A new relationship has been established between the tumor size upon its diagnosis and the prevalence of chest CT under the pandemic conditions of the novel coronavirus infection.
Further study of the genetic characteristics of GISTs, age-related characteristics of the tumor process will allow choosing the best possible treatment regimens for this pathology, increasing the survival rate and reducing the side effects of medical therapy.




















Reference lists